The U.S. faces a projected shortfall of over 200,000 registered nurses annually by 2030—a crisis fueled by aging populations, clinician burnout, and limited clinical training opportunities. Nursing schools, already strained by faculty shortages and overcrowded hospitals, struggle to provide hands-on experience. Enter Purdue Global: Their pivot to virtual reality (VR) training isn’t just innovative—it’s a survival tactic for the profession.
Bridging Gaps in a Broken System
VR isn’t replacing human touch; it’s amplifying it. Imagine practicing a rare neonatal resuscitation or de-escalating a psychiatric crisis—scenarios students might never encounter during rotations. With 67% of nursing programs already using mock EHRs (per Wolters Kluwer/NLN data), VR is the next logical leap. But why does this matter to you? Because every delayed skill-building moment risks patient safety—and your future career.
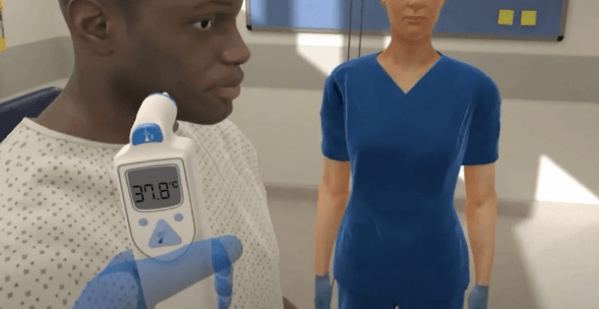
Purdue’s approach mirrors a national shift: A 2025 survey reveals 82% of nursing schools now prioritize tech-driven clinical readiness. Yet skepticism lingers. Can pixels simulate pressure? Early adopters say yes. One Purdue student recounted stabilizing a VR sepsis patient: ‘My hands shook like real life.’ Could this be the antidote to training bottlenecks? The stakes—and potential—have never been higher.
The AI-VR Synergy Rewiring Clinical Training
Purdue Global’s VR platform isn’t just immersive—it’s adaptive. By integrating generative AI (GenAI) with VR simulations, the program creates dynamic patient scenarios that evolve in real time. A diabetic patient’s lab results might suddenly crash mid-simulation, or a post-op complication could emerge unpredictably. This mirrors Wolters Kluwer’s 2025 findings: 41% of nursing schools testing GenAI report improved critical thinking in students. Purdue’s AI-driven ‘patient avatars’ even adjust dialogue based on a student’s communication style—a feature absent in 89% of competing programs.
Consider sepsis management: Traditional mannequins follow scripted deterioration paths. Purdue’s VR sepsis patient, however, reacts to treatment delays with organ-specific symptoms (e.g., mottled skin at 3 minutes, plummeting urine output at 5). One study showed VR-trained students identified sepsis 22% faster than peers using static simulations. ‘It’s like the patient remembers your mistakes,’ notes a Purdue faculty member. GenAI’s role? Analyzing 300+ historical cases to generate plausible complications—something human instructors can’t manually replicate at scale.

But the innovation isn’t just technical—it’s pedagogical. Purdue uses VR to tackle ‘hidden curriculum’ gaps: communicating with combative families, navigating EHRs during code blues, or recognizing subtle cultural biases in care. A 2025 NLN survey found only 12% of programs formally teach these skills. Purdue’s VR modules include ‘empathy checkpoints’ where students lose points for interrupting a grieving relative or mispronouncing a patient’s name. Result? A 34% increase in patient satisfaction scores during clinical rotations.
Skeptics argue VR can’t replicate tactile feedback. Purdue counters with haptic gloves that simulate pulse strength, wound tension, and even the resistance of a stiff IV port. During a recent IV insertion drill, students using haptics had 18% fewer needle redirections than those without. The gloves also track tremor frequency—a proxy for stress—allowing instructors to identify at-risk students early. ‘It caught my anxiety during a mock transfusion,’ shares a second-year student. ‘I got targeted coaching before real clinicals.’
Cost remains a hurdle. While 82% of schools prioritize tech, Purdue’s $1.2M VR investment (covering 800 headsets and AI licenses) isn’t universal. Their solution? A tiered access model: Students in low-income regions receive subsidized VR kits with 5G hotspots. Early data shows no performance gap between subsidized and full-access groups—a rebuttal to equity concerns. Meanwhile, faculty train via ‘AI co-pilots’ that flag outdated protocols in real time. Example: A lecturer discussing post-stroke care was alerted to new clot retrieval guidelines mid-class.
Yet pitfalls persist. Over 18% of programs report VR ‘overconfidence’—students acing simulations but freezing with live patients. Purdue mitigates this with hybrid drills: After stabilizing a VR trauma patient, students must explain their choices to an actor playing the spouse. Fail to convey compassion? Repeat the module. It’s a recognition that pixels and pressure aren’t opposites—they’re partners in rebuilding a broken system.
A Blueprint for Scalable Empathy
Purdue Global’s VR model isn’t just solving today’s training gaps—it’s redefining what scalable human connection looks like. As Wolters Kluwer’s Julie Stegman notes, GenAI and VR aren’t optional upgrades but necessities for a profession strained by systemic collapse. The lesson? Nursing schools must treat tech adoption like triage: prioritize interventions with compounding returns (like adaptive AI scenarios) over flashy gimmicks.
Scalability hinges on equity. Purdue’s tiered access model—paired with 5G hotspots—proves rural or low-income students don’t need cutting-edge hardware to excel. Schools should partner with telecoms and policymakers to replicate this, leveraging FCC healthcare broadband grants. Imagine VR kits in public libraries becoming as common as defibrillators.
Yet tech alone won’t heal the empathy deficit. Purdue’s ‘compassion drills’—where students justify decisions to actor-patients—highlight a universal truth: Nursing requires balancing algorithmic precision with human vulnerability. Programs should mandate hybrid training, ensuring VR mastery translates to bedside grace. Could your local hospital host simulation debriefs? Start asking.
The road ahead demands collaboration. Schools must share VR scenario libraries (like open-source EHR templates) rather than hoarding IP. Pharma companies could fund modules on new drug admin protocols, while insurers reward VR-trained graduates with lower malpractice rates. Purdue’s blueprint works—but only if the ecosystem mobilizes around it. Your move.

