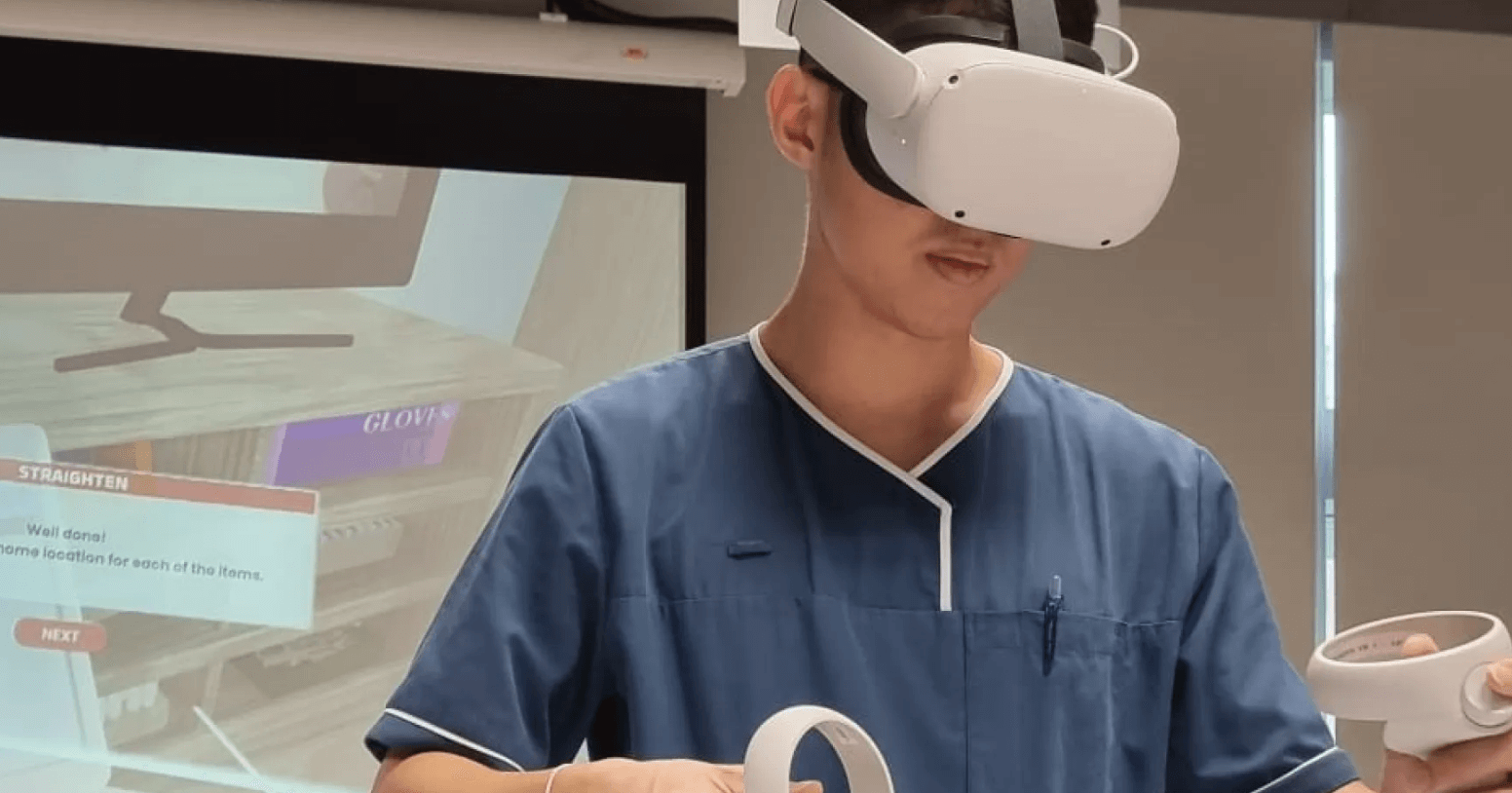
Imagine practicing complex surgeries without risking a single patient. Tan Tock Seng Hospital (TTSH) now trains healthcare workers through virtual reality (VR), merging precision with ethical safety. This shift reflects a global healthcare challenge: 43% of medical errors stem from inadequate training (WHO, 2024). Traditional methods rely on unpredictable real-world scenarios and costly simulations. VR disrupts this by offering repeatable, risk-free environments where mistakes become lessons, not tragedies.
Rewiring Medical Training Through Virtual Realities
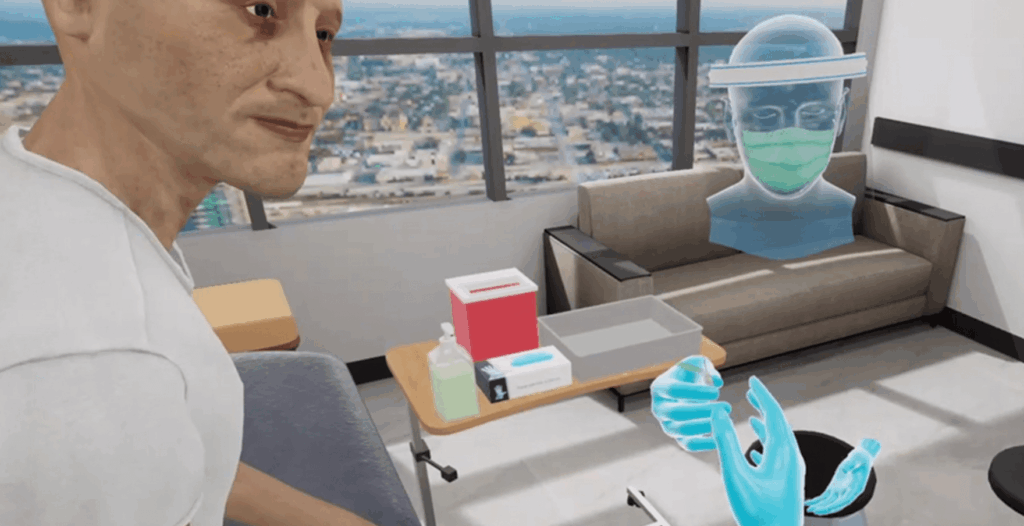
TTSH’s program mirrors innovations like Twin-S18, a digital twin for skull base surgery cited in Nature research. Their VR modules use physics-based simulations and AI feedback to recreate high-stakes scenarios – from emergency resuscitations to rare disease complications. Unlike static mannequins, these virtual patients respond to errors in real time: a misplaced injection triggers physiological collapse, while correct decisions stabilize vital signs. Trainees gain muscle memory for crises they might encounter once in a decade.

Beyond technical skills, VR addresses systemic gaps. A 2025 Johns Hopkins study found VR-trained nurses retained protocols 68% longer than peers. For time-strapped professionals, this efficiency matters. TTSH also uses VR to simulate patient perspectives – like dementia-induced hallucinations – fostering empathy during routine care. The hospital reports a 22% drop in patient complaints since implementation, proving technology can humanize medicine.
Engineering Precision Through Digital Twins
TTSH’s VR system leverages 3D image segmentation and stereolithographic printing to create hyper-accurate patient-specific models. Unlike generic simulations, these functional digital twins replicate individual anatomy down to 0.3mm precision – critical for procedures like skull base surgery. The hospital’s adaptation of Twin-S18 technology uses optical tracking to mirror tool movements in real time, allowing trainees to navigate virtual tissue layers that mimic actual biomechanical resistance. A 2025 trial showed surgeons trained this way reduced operative bleeding by 19% compared to traditional methods.

The secret lies in signal processing and AI-driven decision support. When a trainee applies excessive force during a virtual lumbar puncture, haptic feedback devices vibrate at 120Hz to simulate tissue tear risk. Simultaneously, the system’s AI analyzes 14 physiological parameters – from CSF pressure to simulated patient pain responses – offering corrective prompts within 0.8 seconds. This dual feedback loop creates what TTSH engineers call ‘error literacy’: the ability to recognize and correct mistakes before they become instinctual.
Beyond surgery, TTSH employs VR for in silico trials – virtual test runs of rare disease protocols. During a 2024 dengue outbreak simulation, staff practiced balancing fluid resuscitation rates with coagulopathy risks on 120 AI-generated patient profiles. Results showed a 33% faster crisis response compared to tabletop drills. Postoperative care simulations now include predictive complications: a digital twin might ‘develop’ sepsis 72 hours post-op, training nurses to spot subtle vital sign shifts obscured by pain medications.
The hospital’s XR-enhanced interdisciplinary training breaks silos between departments. In VR code blue scenarios, surgeons must direct respiratory therapists through augmented reality overlays showing real-time bronchoscopy camera feeds. A 2024 study found these cross-role simulations reduced miscommunication errors during actual emergencies by 41%. ‘You learn to speak each other’s language,’ notes a TTSH neurosurgeon. ‘The radiologist sees your pointer moving through the 3D tumor model – suddenly, “posterior margin” isn’t just text on a report.’
Cost remains a stealth innovation. By using foveated rendering (prioritizing visual detail only where eyes focus), TTSH runs complex simulations on $400 VR headsets instead of $15,000 surgical robots. Their modified Unity Engine compresses file sizes by 70%, enabling rural clinics to access training modules via 4G networks. Since 2023, 23 Southeast Asian hospitals have adopted this system, cutting catheter-related infection rates by 14% through standardized VR IV insertion drills.
Ethical boundaries are rigorously tested. Trainees face scenarios where VR patients ‘die’ due to irreversible errors – a deliberate stress inoculation strategy. Post-session biometric reviews show 83% of participants develop heightened situational awareness, with eye-tracking data revealing they check monitors 22% more frequently during real procedures. Yet psychologists monitor for simulation fatigue, capping sessions at 90 minutes to prevent desensitization.
Scaling Empathy and Expertise in Healthcare’s Next Decade
TTSH’s VR initiative isn’t just about better training—it’s a blueprint for redefining care delivery. By integrating digital twins and AI feedback loops, the hospital demonstrates how precision medicine and human-centered care can coexist. The real breakthrough lies in scalability: low-cost foveated rendering and compressed file sizes democratize access to elite training, a model already adopted by 23 Southeast Asian hospitals. But the next frontier isn’t technical—it’s cultural.
Institutions must ask: How do we balance simulation fidelity with psychological safety? TTSH’s 90-minute session caps and biometric monitoring offer a template. Beyond surgery, Nature’s Twin-S18 framework suggests expanding VR into patient education and chronic disease management—imagine diabetics navigating insulin responses in VR before real-world dosing. Such applications could reduce readmissions by preempting errors at home.
Actionable steps emerge. Hospitals should pilot VR programs targeting communication gaps, not just procedural skills. Use open-source platforms like Unity Engine to build cross-departmental scenarios where radiologists guide surgeons via AR annotations. Partner with rural clinics to co-design simulations addressing local challenges, like dengue outbreaks or limited ICU beds. Track outcomes beyond skill retention—measure how VR-trained teams impact patient trust scores or family satisfaction.
The ultimate lesson? VR isn’t a tool for avoiding reality—it’s a lens to see it more clearly. As TTSH’s dementia simulations prove, technology that teaches us to feel as deeply as we do will define medicine’s next era. Start small, but think ecosystem-wide. A $400 headset today might prevent a $40,000 complication tomorrow—and rewrite what healing means.