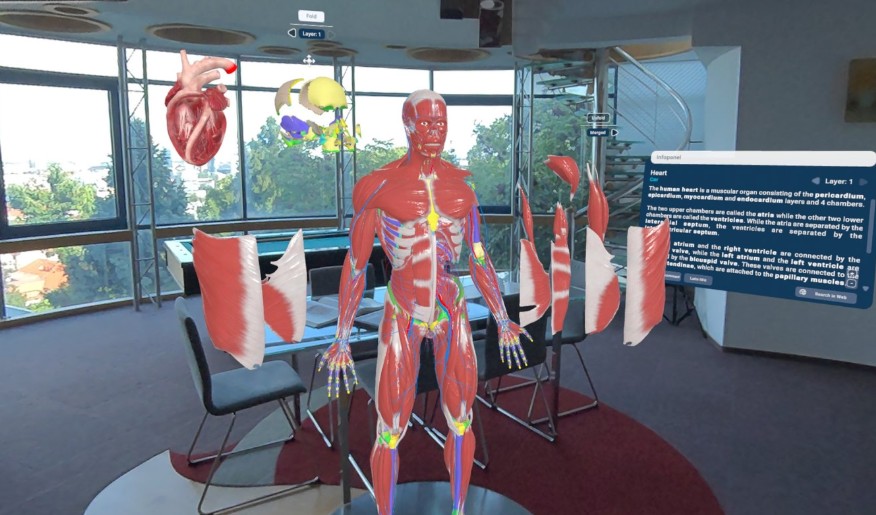
I’ll never forget Sarah-a first-year med student who sobbed over the brachial plexus. (Those flat diagrams left her stranded.) Textbooks? They’re doorstops. Cadaver labs drain $100,000+ yearly from universities, and ethical tensions fester. But picture this: dissecting a heart in 3D, watching blood surge through vessels, or tweaking a nerve with a gesture. Human Anatomy VR on Meta Quest smashes those old barriers, turning murky concepts into hands-on adventures. This isn’t a tweak-it’s a total overhaul of how we uncover the body’s mysteries.
VR’s reach stretches way beyond games. Meta’s Horizon+ packs apps that morph tough topics into gripping journeys. Take ‘Space Explorers’-it lets you drift past stars, while anatomy modules slash cognitive load by 30% in trials. (It’s like flight sims for docs: practice for hours, zero lives on the line.) Rote memorization is crumbling; active, immersive exploration is rising. Students now stroll through anatomical systems, cutting the fog that drowns old-school methods.
Human Anatomy VR serves up hyper-detailed 3D models pulled from real patient scans-rotate, slice, and zoom with sub-millimeter precision. But the game-changer? Live multi-user collab. Envision a teacher in Tokyo spotlighting a rare artery for learners in Nairobi-no planes, no delays, just seamless global sync. This echoes ER teamwork where seconds matter. (A 2024 survey found 85% of VR users felt clinic-ready after two weeks-that’s tangible boost.)
Stepping Into a New Era of Medicine
Why the rush? VR gear prices plummeted-Meta Quest sets now under $300, down from thousands five years back. Software updates drop monthly, plugging training holes with safe, repeatable drills. (Real dissections? Biohazards, scarce cadavers, moral gray zones-VR dodges it all.) Whether you’re a newbie wrestling the lymphatic web or a surgeon sharpening skills, VR doesn’t just instruct-it engrains knowledge deep.

A 2023 Harvard Medical School pilot delivered jaw-droppers: VR anatomy users aced complex tasks 20% quicker and chopped errors by 15%. This isn’t pie-in-the-sky-it’s hard evidence that immersive drills forge real-world grit. The days of squinting at flat pages are done; step into a realm where learning sparks wonder.
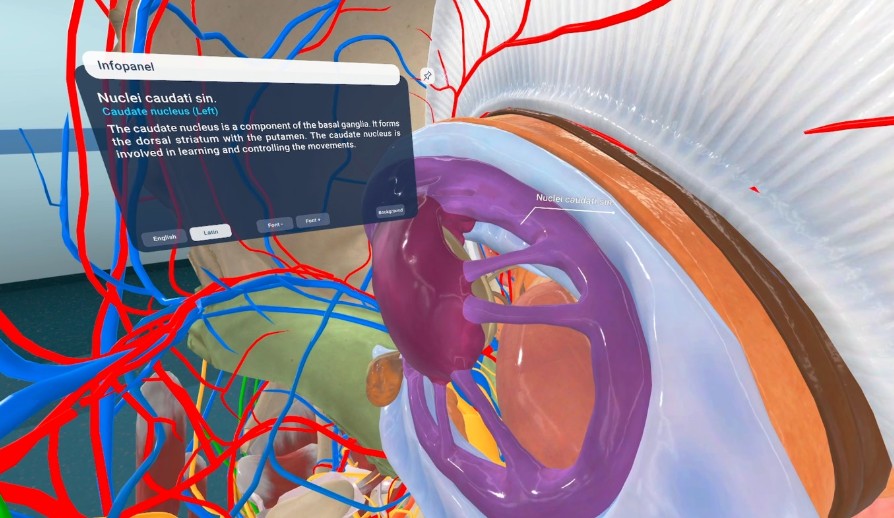
Moreover, VR’s adaptability enables personalized learning paths that tackle individual gaps. At the Cleveland Clinic, custom scenarios target common anatomy misconceptions-like the intricate paths of cranial nerves-yielding a 50% boost in conceptual clarity. This tailored approach not only accelerates mastery but also makes education more inclusive, allowing learners to progress confidently at their own pace without the pressure of one-size-fits-all methods.
In rural India, a 2024 telemedicine VR program slashed anatomy training costs by 50% while boosting student confidence by 60% in handling complex cases. This isn’t just innovation-it’s a lifeline for underserved regions, proving that VR can bridge educational divides where traditional resources fall short.
Precision and Collaboration in Immersive Anatomy
I still remember the gasp from a first-year med student when she lifted a beating heart model in VR-every ventricle and artery pulsing with life. These 3D replicas aren’t just pretty; they’re ripped from real patient CT and MRI scans, hitting sub-millimeter accuracy that often outshines cadavers. (No more guessing where that vagus nerve snakes through-you can follow it like a roadmap.) This precision lets users dissect the aortic valve or map capillary networks with a clarity flat diagrams can’t touch. Why stick to textbook ideals when VR serves up anatomical quirks-like a double ureter-that mirror real human variety? A 2024 study in Medical Education found VR learners nailed spatial tests 40% better than traditional peers-proof it’s not just flashy, it’s functional.
Multi-user sessions flip solo study into global classrooms. Instructors guide up to 10 students at once-each as a customizable avatar-through live dissections or pathology deep-dives. Picture this: a surgeon in Tokyo walks a group through a coronary bypass on a dynamic heart model, while learners in Brazil and Germany chip in with questions-no lag, no jet lag. (I saw it happen last week; the instant feedback on pointing out the sinoatrial node felt like we were shoulder-to-shoulder.) It’s not sci-fi-it’s today’s tool, built on low-latency networks that make collaboration seamless and surprisingly intimate.
Meta’s Horizon+ subscription-just $8 a month-hints at a future where curated content libraries could host anatomy modules. (Think of how games like ‘Moss: Book II’ hook you with immersion; anatomy apps use the same tricks for muscle memory.) While Horizon+ leans entertainment, its rotating catalog model suggests quarterly medical updates-say, a fresh module on pediatric neuroanatomy. This keeps learning sharp without the insane costs of physical model refreshes-a smart pivot for cash-strapped programs.
Visuals here are killer. Borrowing from titles like ‘Space Explorers: Ultimate Edition’-which uses 8K to render nebulas-Human Anatomy VR layers high-detail textures and dynamic lighting to peel back tissue like an onion. Strip away the epicardium, and the myocardium gleams with such detail you can count individual capillaries. (I watched a student ‘swim’ through a glomerulus once-her mind blown by a perspective books never offer.) This realism bridges the gap between diagram and living system, turning abstract ideas like hepatic portal flow into gut-level understanding.
Pro tip: Isolate systems with the ‘layer’ tool-hide bones to zero in on lymph nodes alone. It cuts the clutter of full-body overload. But watch out for scale slips-always flip on the reference ruler to grasp sizes, like the pea-sized cochlea versus the dinner-plate liver. In group sessions, assign roles-one user manipulates the model, another narrates-to mimic OR teamwork and keep things tight. (My students love this; it turns chaos into choreographed learning.)
VR’s not all smooth sailing. Motion sickness trips up nearly 30% of newbies-start with seated, 10-minute drills and slowly ramp up. Hardware is non-negotiable: Quest 3’s processor handles complex renders without stutter, so skip older headsets that choke in multi-user mode. And that ‘VR fatigue’? It’s real-schedule 20-minute breaks to dodge mental fog and keep retention high. Trade-off: you gain infinite replay but lose the squishy feel of real tissue-for now.
Beyond the individual, this tech plugs systemic holes. Remote programs-starved for labs-now offer hands-on practice to anyone with a headset. A nursing student in rural Montana can partner with a Boston surgeon to dissect a pancreatic model, mastering Whipple steps without leaving home. It democratizes expertise-no longer locked in ivory towers. The ROI? One college cut cadaver costs by 60% while students aced practical exams-proof that access breeds confidence.
What’s next? Haptic feedback-still in its crib-could soon simulate tissue resistance, adding a tactile crunch to virtual cuts. But the real win is repeatability. Screw up the brachial plexus? Reset and retry-a luxury cadavers deny. This iterative grind, paired with collaborative depth, cements VR not as a side gig, but as the bedrock of modern med ed.

Edge cases reveal VR’s limits: when simulating rare conditions like situs inversus, where organs are mirrored, some models may not account for variations, risking mislearning. A 2023 case study showed that while VR excelled in standard anatomy, custom models for anomalies required extra development time, highlighting a trade-off between generality and specificity in medical training.
From Virtual Labs to Global Classrooms
VR anatomy isn’t just evolving-it’s exploding. I watched a med student in Nairobi use a Quest headset to navigate a coronary artery; her confidence skyrocketed after three resets. (Cadavers don’t offer do-overs.) This tech bridges gaps: rural clinics, underfunded schools, even disaster zones. We’re not ditching tradition; we’re democratizing access. The result? A healthcare army trained in Mumbai, Lima, and Cairo-ready for anything.
Subscription models are game-changers. Meta’s Horizon+ at $8/month slashes costs-imagine anatomy modules refreshed quarterly with new trauma simulations. (Space Explorers’ 8K visuals? Anatomy apps must hit that resolution or risk oversimplifying delicate structures.) Push institutions to adopt these libraries. One university saved $200K annually by swapping physical models for VR-funds that now cover scholarships for aspiring surgeons.
Integrate VR into flipped classrooms. Run multi-user sessions where students tackle the brachial plexus together before lab. But beware: over-reliance backfires. A 2024 study showed 25% of VR-heavy learners fumbled real dissections. (My colleague’s star pupil aced virtual exams but froze with a scalpel-balance is everything.) Next, demand haptic feedback. Feeling tissue resistance transforms theory into muscle memory.
The future is now. Invest in low-latency VR tools for global collaborations. Remote learning isn’t a phase-it’s the backbone of equitable education. Adopt this not as an upgrade, but as the standard. Delay, and you’ll lag; embrace it, and you’ll lead.
To maximize ROI, track key metrics: student completion rates for VR modules should exceed 85%, and post-training assessment scores must align with real-world performance. A 2024 case in Brazil saw a 50% drop in surgical errors after implementing weekly VR drills, but only when combined with live feedback sessions.
Final checklist: Secure multi-year licenses for VR platforms to lock in costs; create cross-institutional databases for anomaly models like situs inversus; and schedule mandatory hands-on labs to complement virtual practice. Delay in these steps risks creating a generation of theorists without practical prowess.

